January 2024
Are You Suffering From Ingrown Toenails?
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
Types and Symptoms of Foot Arthritis
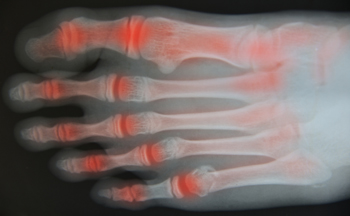
Foot pain can be a common issue, often arising from various causes, such as sports activities, prolonged standing at work, or wearing ill-fitting shoes. It can range from minor discomfort to debilitating pain, and its roots can be diverse. Overuse, strain on tendons or ligaments, fractures, or arthritis are some of the contributing factors. Arthritis can significantly impact foot health. Osteoarthritis, or OA, the most common type, can affect the foot's 33 joints, leading to pain and misalignment. Rheumatoid arthritis, or RA, an autoimmune form, often starts in small hand and foot joints, causing pain and swelling. Psoriatic arthritis, or PsA, affects skin and joints, causing unique issues like dactylitis and plantar fasciitis. Gout, characterized by uric acid crystals, can cause sudden, intense pain, generally in the big toe. In systemic lupus erythematosus, or SLE, foot pain is often overlooked. Lupus-related arthritis, muscle, nerve, and soft tissue issues can lead to foot problems. Immunosuppressant medications increase the risk of complications, making proper footwear and podiatric care vital for lupus patients. If you have foot pain of any sort that is not a one-time issue, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Bazzi Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck, Dearborn Heights, Madison Heights, Redford, and Livonia, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
Symptoms and Treatment of Plantar Warts

Plantar warts, caused by the human papillomavirus, or HPV, are thick, rough skin growths found on the bottom of the foot. While they are benign, the discomfort they can cause is far from trivial. Plantar warts typically form on pressure points such as the heel or ball of the foot, entering the skin through cuts or scratches. Direct contact with an infected surface or person can also lead to their development. Treatment options include keratolytic therapy, cryotherapy, immunotherapy, and laser therapy. In severe cases, surgery is needed. Keratolytic therapy employs acid medication to thin the wart, prompting the outer skin layer's shedding. Cryotherapy involves freezing the wart with liquid nitrogen, creating a red blister that eventually leads to the wart's natural removal. Immunotherapy, using creams or shots, enhances your immune system to combat HPV and eliminate the wart. Laser therapy utilizes focused light to cut away the wart, while surgical removal, performed by numbing the skin and burning the area, becomes necessary in some cases to prevent recurrence. If you have been infected with plantar warts, it is suggested that you schedule an appointment with a podiatrist who can examine your foot and suggest the treatment option that is best for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Bazzi Podiatry. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck, Dearborn Heights, Madison Heights, Redford, and Livonia, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Choosing the Right Running Shoe
Choosing the right running shoes for you is an important part of running. A good pair of running shoes will make the running experience more enjoyable for you and prevent potential injury.
Poorly-fitted shoes can increase the risk of injury in runners substantially. Common injuries from running with poor quality shoes include shin splints, sprained ankles, Achilles tendinitis, stress fractures, plantar fasciitis and more. This is due to the fact that bad shoes do not provide proper foot support, can increase pronation (how much the foot rolls when hitting the ground), have little to no cushioning, do not allow the feet to breath, and do not provide enough flex and rigidity in the right parts.
When looking for running shoes, first, determine where you will be running. If you are a trail runner, then pick trail shoes. If you run on concrete and asphalt, then regular running shoes are the best choice. When trying on shoes, its best to go at the end of the day as feet grow during the day and shrink after a night of sleep. Shoes should be more rigid towards the back of the foot while being more flexible up where the toes are. The toe box should provide enough room for the toes to move freely. The overall fit should be snug, not too tight but not too loose. A good pair of running shoes should also provide enough arch support for your foot type. If you experience overpronation or under-pronation while running, try to find a pair of shoes that will help correct this with different sole patterns. Finally, try to find a pair of shoes that allow the feet to breathe like nylon mesh or synthetic leather.
Don’t forget about the socks either. Socks that hold too much moisture can lead to athlete’s foot. Socks should be breathable so that your feet can air out and breathe. Synthetic socks wick away moisture like sweat. If you tend to run a lot, having a second pair of shoes that you can wear while you let the first pair air out is smart. Just don’t forget to replace your shoes after about every 300 to 500 miles.
Before you start running, it is advised to see a podiatrist to see if running is right for you. They can also offer good advice on how to run and what to look for in a pair of running shoes. If you have flat feet or poorly supported ones, they can also offer custom-made orthotics that will help give your feet the support they need.
How to Choose Shoes for Distance Running

Embarking on the journey of distance running necessitates a discerning choice in footwear, an essential companion for every stride. Wearing the right distance running shoes is one of the ways to avoid injuries. Designed with meticulous precision, distance running shoes are crafted to endure the relentless rhythm of long-haul runs. These shoes seamlessly blend support and cushioning, striking an equilibrium that cradles the foot through each mile. The robust yet lightweight construction becomes a symbiotic extension of the runner, mitigating impact and maximizing efficiency. Breathable materials envelop the foot, ensuring comfort and ventilation. The soles, engineered for durability, provide a reliable grip on the terrain beneath, enhancing stability and confidence. If you require additional information about the right type of shoe for your running needs, it is suggested that you consult a podiatrist.
You should always make sure your running shoes fit properly in order to avoid injury. For more information, contact one of our podiatrists from Bazzi Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
Improper shoe sizing can cause a myriad of problems for your feet. Shoes that don’t fit you properly can lead to muscular imbalances in your body, which can result in foot, knee, and hip injuries.
Tips for Finding the Right Running Shoe
- Make sure you have a thumb’s width of wiggle room between the end of your longest toe and the front of the shoe.
- There should be little to no slipping at the heel
- Don’t assume your size in one shoe brand will be your size in another
- Do not lace up your shoes too tightly
- Walk around in the store with your new shoes before you buy them
If you have any questions please feel free to contact our one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck, Dearborn Heights, Madison Heights, Redford, and Livonia, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treatment Options for Stress Fractures

Treatment options for stress fractures focus on promoting healing, managing pain, and preventing complications associated with these injuries. Stress fractures typically result from repetitive stress or overuse and require careful attention to facilitate recovery. Rest is a fundamental component, involving the reduction or avoidance of activities that led to the fracture, allowing the affected bone to heal without additional strain. In some cases, immobilization with the use of casts, braces, or walking boots may be necessary to support proper healing. Modifying weight-bearing activities can also alleviate stress on the fracture site, often requiring the use of crutches or assistive devices. Pain management strategies may involve medications to address discomfort and inflammation. Wearing custom orthotic devices or shoe inserts may offer better support and alignment for the affected area, reducing bone stress. Adjusting activity routines, incorporating appropriate warm-up and cool-down exercises, and avoiding excessive exertion are essential in preventing future stress fractures. A balanced diet with sufficient calcium and vitamin D supports bone health and healing. While surgery is rarely needed, it may be considered when conservative treatments prove ineffective at stabilizing the bone. If you have sustained a stress fracture in your feet or ankle, it is suggested that you schedule an appointment with a podiatrist for an evaluation and personalized treatment plan.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from Bazzi Podiatry. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck, Dearborn Heights, Madison Heights, Redford, and Livonia, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.