January 2022
Heel Pain Is Often Caused by Plantar Fasciitis
The plantar fascia is a thick band of tissue on the bottom of the foot that connects the heel with the forefoot. Because the plantar fascia is so instrumental in the mechanics of walking, it can become overloaded and stressed from overuse, excess weight, structural issues in the foot, or improper footwear. This strain can cause the plantar fascia to become excessively stretched, painful and inflamed. Tiny tears may also develop in the tissue, particularly where it connects with the heel bone. This condition is known as plantar fasciitis. The pain of plantar fasciitis tends to be worse in the morning or after periods of rest, and may lessen as you move around and warm up. Wearing footwear with insufficient support in the heel or walking barefoot can intensify the pain. If you believe you may have plantar fasciitis, it is important to seek the care of a podiatrist as soon as possible to treat the condition before it worsens.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Bazzi Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck and Dearborn Heights, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
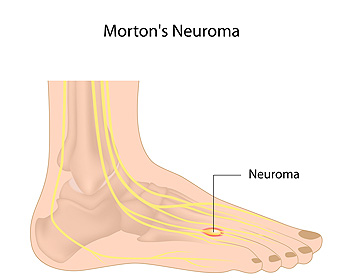
Why the Ball of Your Foot Feels Like It Is on Fire
Morton’s neuroma occurs when the tissue surrounding a nerve in the toes thickens in response to the nerve becoming entrapped, or otherwise irritated. This usually occurs between the third and fourth toes, however, it can also occur between the second and third toes. Morton’s neuroma can cause a burning pain in the ball of the foot. People with this condition sometimes explain the pain they feel as walking on a pebble or having a bunched-up sock in the front of their shoe. The toes may also feel numb or tingling, and there may be difficulty walking. Wearing shoes that are too tight or that compress your toes may sometimes contribute to the formation of Morton’s neuroma. This can include ski boots and ballet slippers too. Other foot dysfunctions that squeeze or put pressure on the toes can be contributing factors, such as flat feet, bunions, hammertoes, and high arches. Certain repetitive sporting activities may also be responsible. If you ever experience any of the symptoms mentioned here, call a podiatrist. They will examine you and run diagnostics to rule out other possible conditions and create a treatment plan to relieve pain and treat the underlying thickened tissue and nerve compression.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Bazzi Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck and Dearborn Heights, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Signs of Peripheral Artery Disease
 A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Bazzi Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck and Dearborn Heights, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Reminder: When Was the Last Time...?
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
What You Need to Know About Broken Toes
 Broken toes often result from trauma. They may occur from dropping something directly on the toes, stubbing a toe, or bending them the wrong way. Toes can also break due to a stress fracture after a sudden increase in activity. The common indications of a broken toe include a snapping or popping sound at the time of the injury, swelling, bruising, and pain that becomes worse when the toe is moved. Patients who notice these symptoms may have a broken toe and would be wise to see a podiatrist who can assess the injury. A podiatrist will need to take an x-ray, and if a broken toe is confirmed, they can determine the best course for treatment. Depending on the nature of the break, the toe can be “buddy-taped” to the uninjured toe next to it, placed in a cast, or in severe cases surgery may be required.
Broken toes often result from trauma. They may occur from dropping something directly on the toes, stubbing a toe, or bending them the wrong way. Toes can also break due to a stress fracture after a sudden increase in activity. The common indications of a broken toe include a snapping or popping sound at the time of the injury, swelling, bruising, and pain that becomes worse when the toe is moved. Patients who notice these symptoms may have a broken toe and would be wise to see a podiatrist who can assess the injury. A podiatrist will need to take an x-ray, and if a broken toe is confirmed, they can determine the best course for treatment. Depending on the nature of the break, the toe can be “buddy-taped” to the uninjured toe next to it, placed in a cast, or in severe cases surgery may be required.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact one of our podiatrists from Bazzi Podiatry. Our doctors will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact one of our offices located in Detroit, West Detroit, Northwest Detroit, Sterling Heights, Hamtramck, Dearborn Heights, and Madison Heights, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.